Briefly Describe the Steps in Bone Deposition
The osteocyte continues to secrete. On the flip side of the coin osteoclasts also affected by the piezoelectric effect or unloading do their work of removing bone materials in regions of reduced compressional stress.
Up to 24 cash back The cranial bones undergo.

. This is the fracture hematoma stage. Describe the steps involved in bone repair. The osteoblasts secrete collagen fibers and other organic substances to begin formation of matrix.
Once activated the osteoclasts can secrete various enzymes including collagenases that are capable of digesting the mineralized bone and its collagen. They continue to change over the course of a lifespan. PTH increases the activity of osteoclasts to increase bone resorption which ultimately increases Ca2 in blood.
In step three a bony callus is formed. The blood solidifies to form a clot which reduces bleeding. Describe the steps in bone repair.
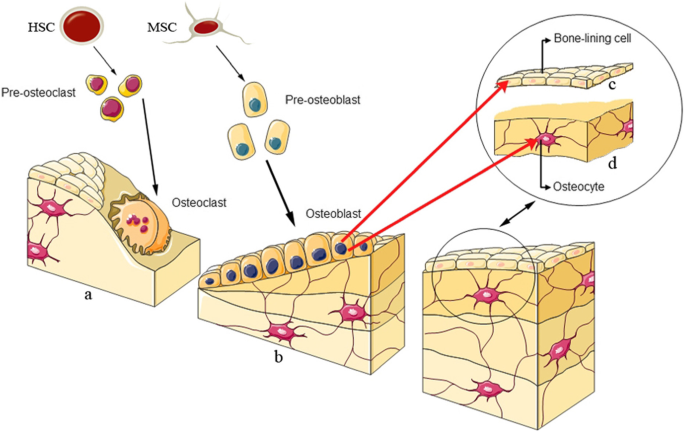
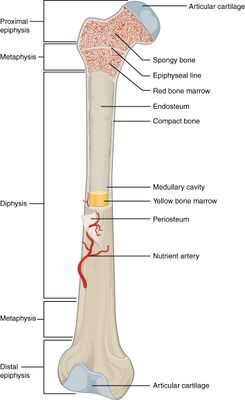
The diagram illustrates repair of a bone fracture. The osteoblast in its new lacuna is isolated and becomes an osteocyte. Bone deposition is the addition of minerals and collagen fibers to bone by osteoblasts.
Within the spaces between fibers calcification occurs toform a solid matrix that eventually surrounds the osteoblast and some extracellular fluid. During bone deposition osteogenic cells develop into osteoblasts. Bone remodeling involves the removal of mineralized bone by osteoclasts followed by the formation of bone matrix through the osteoblasts that subsequently become mineralized.
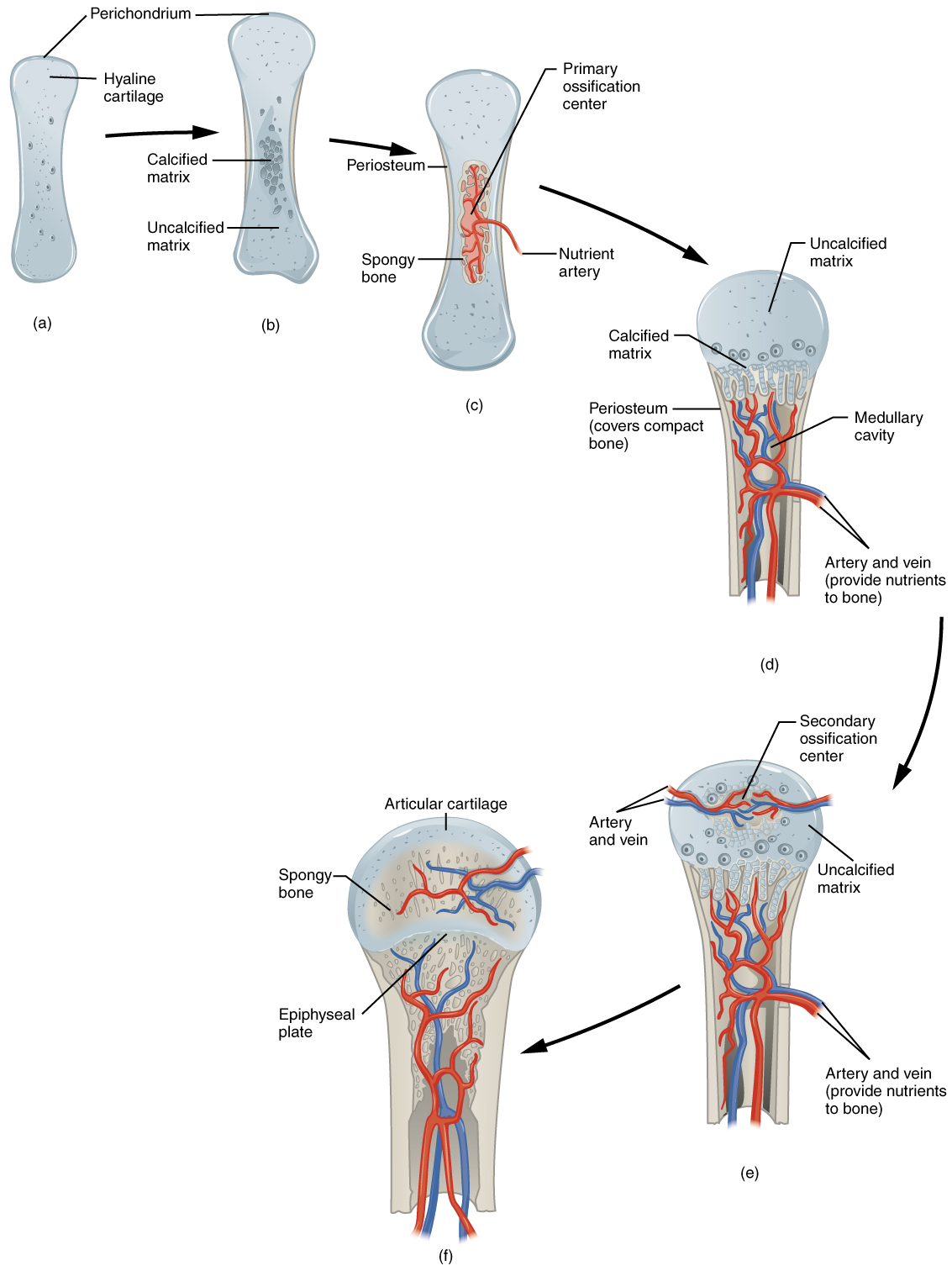
Figure 642 Endochondral Ossification. Bone resorptiondissolution of hydroxyapatite produced by the action of osteoclastsfig. During bone deposition osteogenic cells develop into osteoblasts.
D Endochondral ossification where fibrous tissue is replaced with bone. When a broken bone is manipulated and set into its natural. C Capillaries penetrate cartilage and.
Osteoclastic resorption occurs by secretion of acid and proteolytic enzymes which digest the bone matrix. Endochondral ossification follows five steps. In step two a fibrocartilaginous callus is formed.
Briefly describe the processes by which bone increases in length and diameter. Hydroxyapatite crystals are deposited into the bone matrix. After the break in the bone occurs blood vessels in that area are damaged and blood surrounds the fracture.
Swelling and inflammation may also occur during this time as response to nearby bone cells dying. Within the spaces between fibers calcification occurs to form a solid matrix that eventually surrounds the osteoblast and some extracellular fluid. B Intramembranous ossification where fibrous tissue is replaced with bone.
A Mesenchymal cells differentiate into chondrocytes that produce a cartilage model of the future bony skeleton. Calcification of bone occurs when calcium and phosphate ions move out of the blood into the bone tissues. This process of skeletal change is known as bone remodeling which both protects the structural integrity of the skeletal system and metabolically contributes to the bodys balance of calcium and phosphorus.
1 After the break in the bone occurs blood vessels in that area are damaged and blood surrounds the fracture. It will heal whether or not a physician resets places it in its anatomical position. A Intramembranous ossification where cartilage is replaced with bone.
1918a results in the return of bone calcium and phosphate to the blood. A fracture is a broken bone. Ca2 and PO43- are then taken up by the osteoclasts and released into the circulation.
In step four bone remodeling begins. Remodeling entails the resorption of old or. PTH also stimulates the production of calcitriol which acts on the GI tract to increase absorption of Ca2 from the.
2 WBC migrate into the area to remove bacteria and damaged cells. The reparation of the bone occurs in 4 steps. C Endochondral ossification where cartilage is replaced with bone.
Ridges in periosteum create groove for periosteal blood vessels in step one of bone deposition. White blood cells migrate into the area to remove bacteria and damaged cells. It takes 6-8 hours to form this.
First the formation of fracture hematoma is the process where the blood from the broken blood vessels leaks and forms a clot at the site of fracture. When blood Ca2 levels drop PTH is secreted from the parathyroid glands. If the bone is not reset correctly the healing process will rebuild new bone but keep the bone in its deformed position.
Bone resorption begins when the osteoclast attaches to the bone matrixand forms a ruffled membrane see fig. In the second step of bone deposition periosteal ridges fuse forming an endosteum-lined tunnel. In step one there is formation of a fracture hematoma.
PTH also acts on the kidneys to prevent Ca2 loss in the urine. Now in the interstitial fluid the products of bone resorption diffuse into nearby blood capillaries. Describe the steps in bone repair 1 Formation of fracture hematoma- blood leaks from the torn ends of blood vessels a clotted mass of blood forms around the site of the fracture 2 Fibrocartilaginous callus formation- Fibroblasts invade the fracture site and produce collagen fibers bridging the broken ends of the bone.
The osteoblasts secrete collagen fibers and other organic substances to begin formation of matrix. The blood becomes solid to form a clot which reduces bleeding. The osteoblasts secrete collagen fibers and other organic substances to begin formation of matrix that eventually surrounds the osteoblast and some extracellular fluid.
The degraded bone proteins and extracellular matrix minerals enter an osteoclast by endocytosis cross the cell in vesicles and undergo exocytosis on the side opposite the ruffled border. Bones are not inert structures within the human body. During bone deposition osteogenic cells develop into osteoblasts.
B Blood vessels on the edge of the cartilage model bring osteoblasts that deposit a bony collar. It results in the formation of bone extracellular matrix. This process is called bone deposition.
During this first step many preosteoclasts mature into osteoclasts which are able to de-mineralize the bone. Bone formation occurs by osteoblasts secreting an organic matrix osteoid and then mineralizing the matrix.
Application Of Decellularized Bone Matrix As A Bioscaffold In Bone Tissue Engineering Journal Of Biological Engineering Full Text
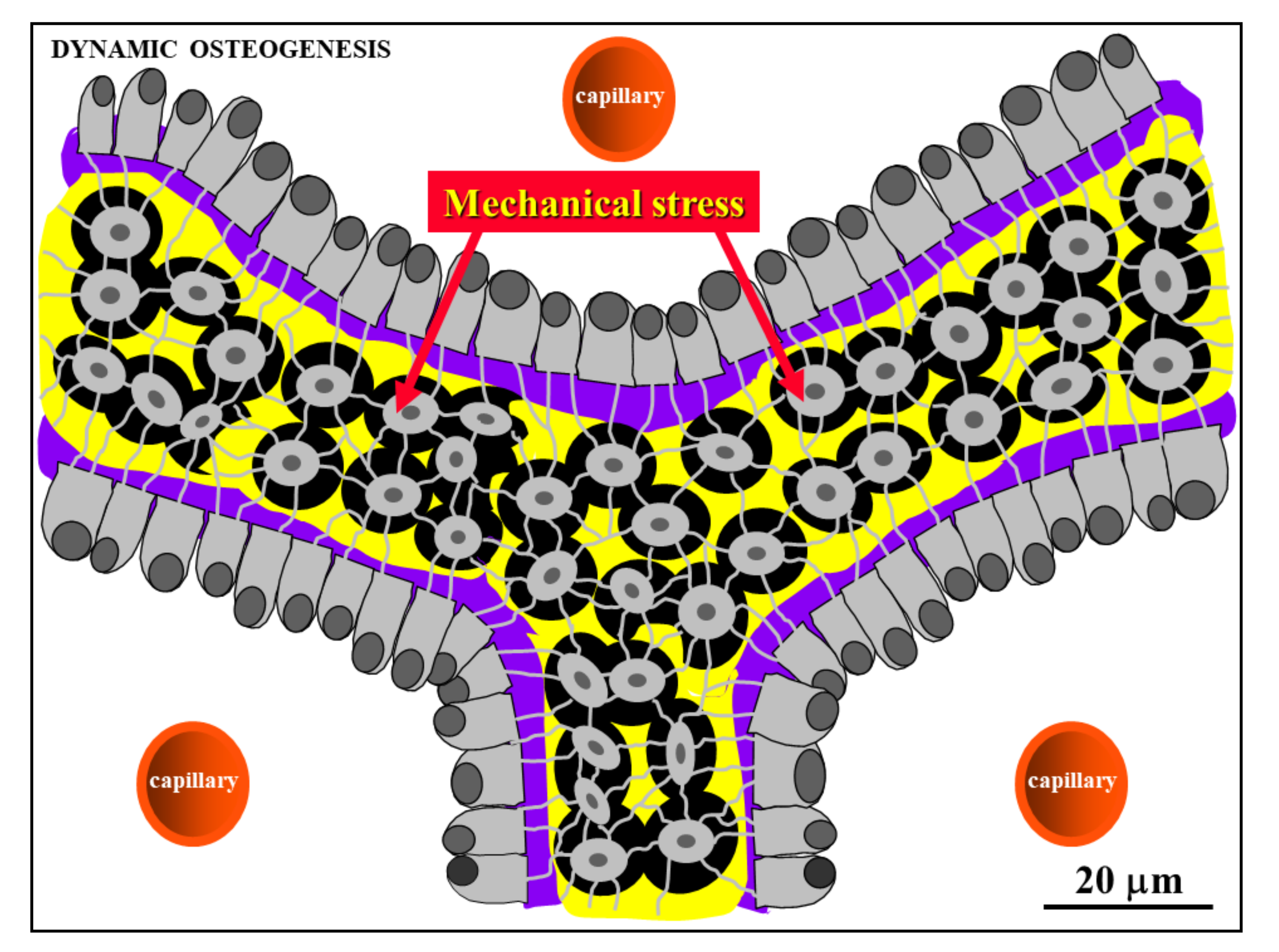
Applied Sciences Free Full Text Static Osteogenesis Versus Dynamic Osteogenesis A Comparison Between Two Different Types Of Bone Formation Html
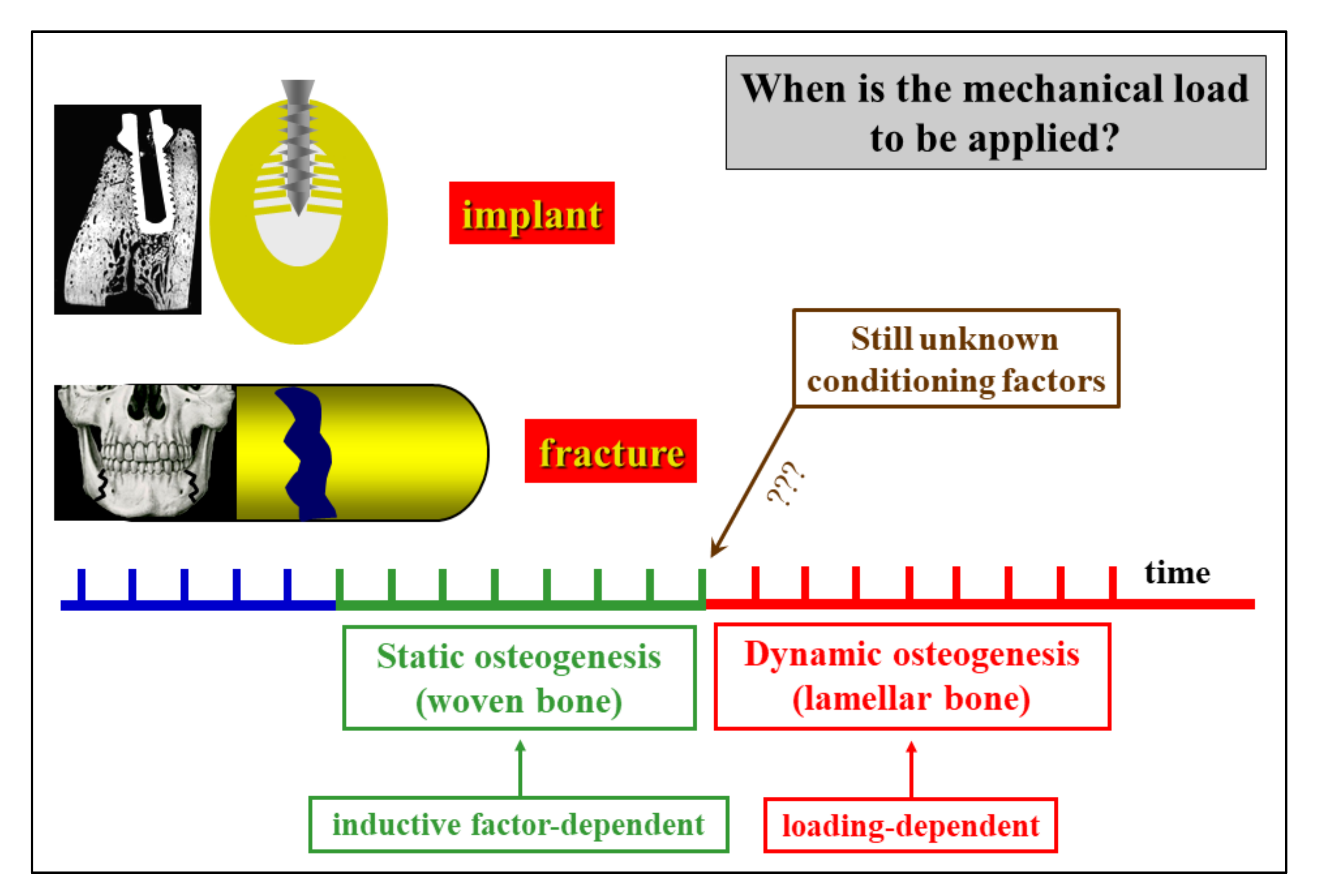
Applied Sciences Free Full Text Static Osteogenesis Versus Dynamic Osteogenesis A Comparison Between Two Different Types Of Bone Formation Html

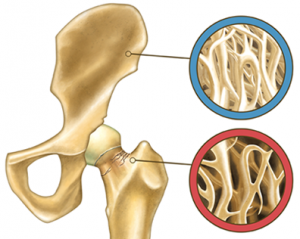
Skeletal System 1 The Anatomy And Physiology Of Bones Nursing Times

Pdf A Multidisciplinary Journey Towards Bone Tissue Engineering

Role Of The Osteoclast In The Mechanism Shifting Bone Remodeling Download Scientific Diagram
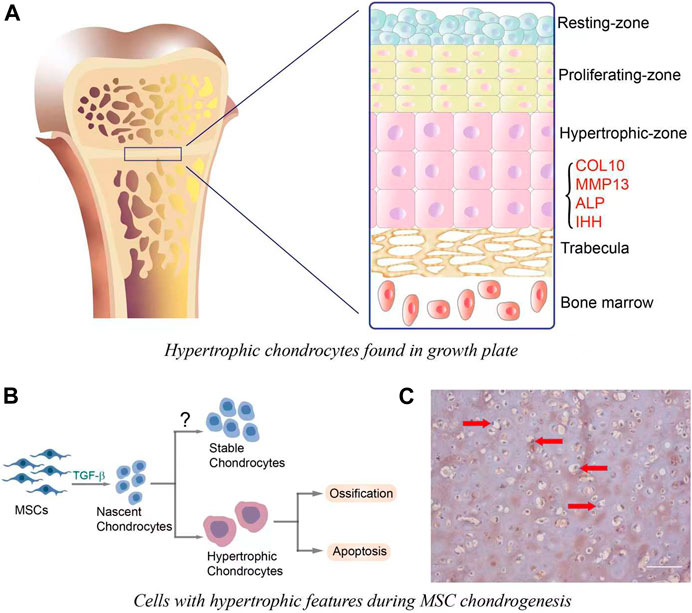
Frontiers Role Of Canonical Wnt B Catenin Pathway In Regulating Chondrocytic Hypertrophy In Mesenchymal Stem Cell Based Cartilage Tissue Engineering Cell And Developmental Biology

Bone Tissue An Overview Sciencedirect Topics
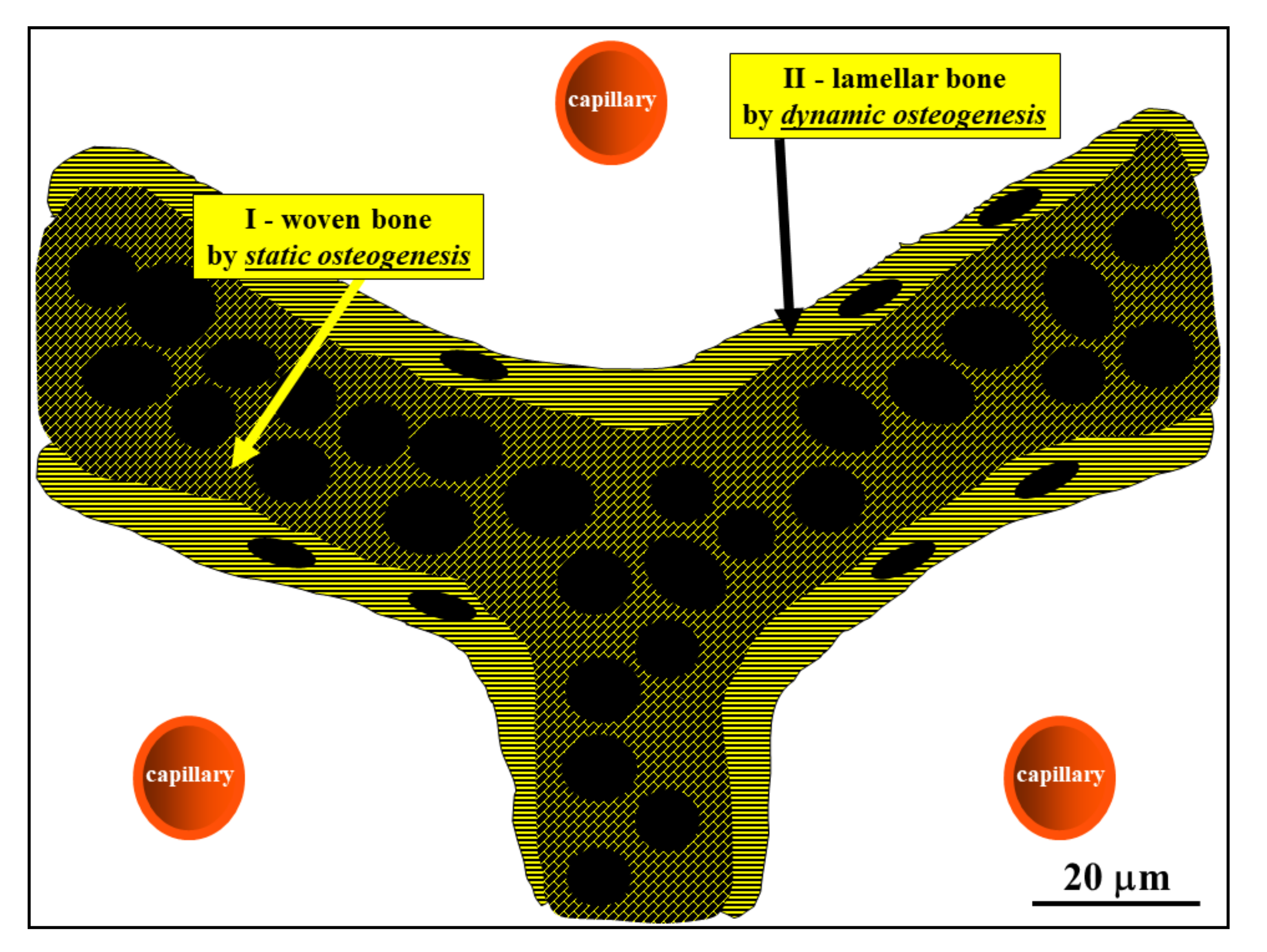
Applied Sciences Free Full Text Static Osteogenesis Versus Dynamic Osteogenesis A Comparison Between Two Different Types Of Bone Formation Html

Applied Sciences Free Full Text Static Osteogenesis Versus Dynamic Osteogenesis A Comparison Between Two Different Types Of Bone Formation Html

Bone Types Of Bone Formation Britannica
Bone Formation And Development Anatomy And Physiology
Bone Resorption Mybiosource Learning Center
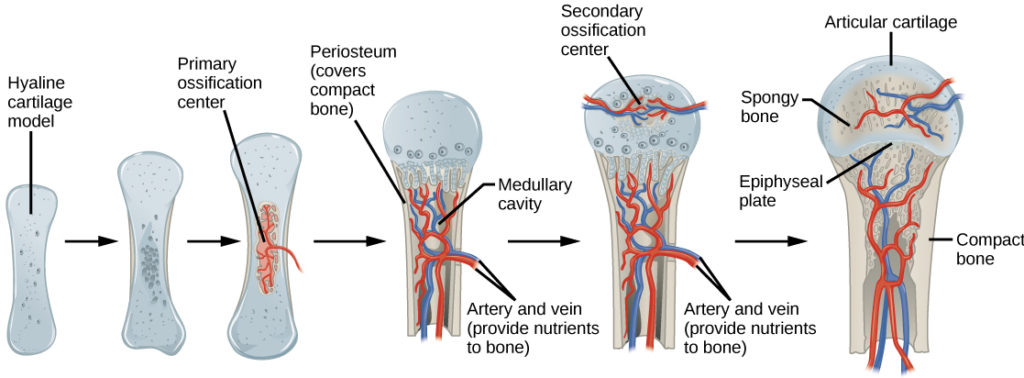
Bone Growth And Development Biology For Majors Ii

Bone Formation Definition Physiology Britannica

Bone Remodeling Physiology Britannica

Ijms Free Full Text From Stem Cells To Bone Forming Cells Html

Bone And Tooth A The 9 Hierarchical Levels Of Bone As Determined By Download Scientific Diagram

Comments
Post a Comment